Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Evolution of Technology in the Management of Early Stage (T1) Cancer of the Glottic Larynx, an Institutional Review of Radiation Therapy Outcomes
*Corresponding author: Jim Wright, MD, Division of Radiation Oncology, Juravinski Cancer Centre, Hamilton Health Sciences, 3rd Floor 699 Concession St, Hamilton, ON L8V 5C2, Canada, Tel: +1(905) 5212100; Fax: +1 (905) 575-6326; Email: wrightjim@hhsc.ca
Received: October 17, 2022; Published:October 21, 2022
DOI: 10.34297/AJBSR.2022.17.002341
Abstract
Purpose: This single institution, retrospective cohort study was undertaken to evaluate the impact of evolving radiation therapy
(RT) treatment technology on the long-term outcomes and patterns of failure for patients with early stage, T1, squamous cell cancer
of the larynx.
Materials and methods: All patients with T1N0 squamous cell cancer of the larynx that underwent radical RT from January 2008 to
December 2018 were included. The planning and delivery of radiation, 2-dimensional RT vs IMRT or VMAT, as well as patient factors
were reviewed in the context of local disease control.
Results: A total of 171 Patients were eligible for inclusion in the analysis. The median age was 70 years (range of 38-91 years), and
just over 90% (90.6%) of the cohort were male. While all patients were staged as having T1 disease, a smaller proportion had more
detailed assignments of T1a (38 or 23.3%), or T1b (23 or 14.1%). The majority of patients were treated with 50-51 Gy in 20 daily
fractions over four weeks. After a median follow up of over five years, there were only 11 patients (6.4%) that had demonstrated
local regional failure, most occurring within the first two years of follow up, and in a multivariate model, only age was a prognostic
factor for local control (p=0.013), whereas RT technique specifically was not.
Conclusion: Single-modality RT provides an excellent and effective treatment for T1 glottic cancer. A shift to conformal 3-D planning
and treatment delivery to minimize radiation dose to surrounding normal tissues, has not resulted in a significant change to rates
of local failure. The majority of local failures have occurred within the first 2 years after RT. Prospective comparative measures of
toxicity and functional preservation seem unlikely to be measured given the shift in the routine delivery of RT.
Keywords: Radiation Therapy; VMAT; Early Stage (T1); Larynx Cancer; Squamous Cell Carcinoma of the Larynx
Introduction
Squamous cell carcinoma (SCC) of the glottis is the most common form of laryngeal cancer and early-stage disease generally has a favorable prognosis. Tumors arising on the true vocal cords typically result in hoarseness leading to early diagnosis, and the incidence of positive lymph nodes for T1-2 glottic is low due to minimal lymphatic drainage [1,2]. Treatment options may include transoral laser excision, open partial laryngectomy and radiotherapy (RT) [3,4]. Based on the favorable prognosis associated with this early-stage cancer, the aim of treatment includes both optimizing local control and maximizing the preservation of laryngeal function. Historical data have reported five-year local control rates of over 90% and likewise, cause specific survival at five years is also quoted at over 90% for RT alone. Studies have shown that local control is better with higher doses per fraction, specifically when 225 cGy/ fraction is used. Mendenhall et al. [5], quoted local control of 95 %, Wong et al. [6] reported 93 % local control with RT, and Warde et al. [7] reported a range in local control of 82-91% in patients with stages T1a-T1b respectively.
During the past decade there have been technological advances in the planning and delivery of routine RT [8-10]. But as is often the case, the rigor of clinical assessments to evaluate these technologic changes has lagged the implementation. The compelling rationale for newer RT techniques includes the lower dose of radiation to normal structures, such as the contralateral vocal cord, and the carotid arteries but the inherent risk of a more targeted approach is the higher risk of a geographic miss, especially with a malignant burden as small as early-stage larynx cancer [11,12]. Most of the available evidence as outlined previously reported outcomes based on the use of historical 2D techniques of RT delivery. More recent reports of smaller cohorts have begun to report the results of disease control with newer planning and treatment techniques including Intensity Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT). In a recent publication [13], a cohort of 153 patients treated with conventional 2D treatment had locoregional control of 94% vs 62 patients treated with IMRT which had local control of 97%, both at three years. This difference was not statistically different.
Likewise, IMRT for the treatment of T1-T2 glottic cancer was evaluated by Zumsteg et al. [14] and no differences in the rate of local failure were found in comparison to conventional RT. Three years local control rates were reported as 88% vs 89%, with carotid sparing IMRT versus conventional RT respectively.
Since June 2015 patients with early-stage larynx cancer at our center have routinely been treated using VMAT or IMRT. Hence, this presents an opportunity to evaluate the outcomes of this group of patients treated with newer techniques (VMAT and IMRT) over a period of time which saw the evolution to the routine use of these techniques.
Materials and Methods
This study represents a single-institution, retrospective cohort review performed at the Juravinski Cancer Centre (JCC) Hamilton, Ontario. The JCC is a tertiary cancer center which covers a population of 1.4 million people in the south-central part of Ontario, Canada. The study was approved by our local research ethics board. Patients within this cohort were initially evaluated clinically as part of our multidisciplinary head and neck clinic with collaborative staging conducted by both surgeons and radiation oncologists. A patient with pathological evidence of only Tis could be upstaged to T1 based on the clinical evaluation performed by the radiation oncologist and surgeon without subsequent tissue confirmation of invasiveness.
Patient Eligibility
Between January 2008 and December 2018, 171 patients with pathologically proven SCC, staged as clinical T1, of the true vocal cords that underwent definitive RT at the JCC were included in this analysis. All patients had documented local disease status as part of their routine clinical follow-up, and most were followed with clinical evaluations for at least five years following the completion of treatment.
Radiation Therapy
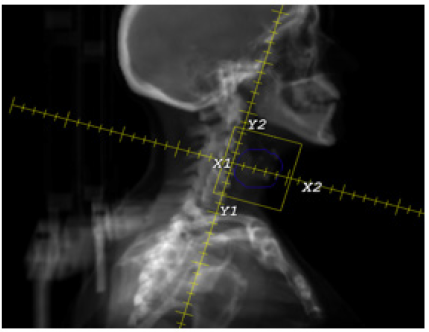
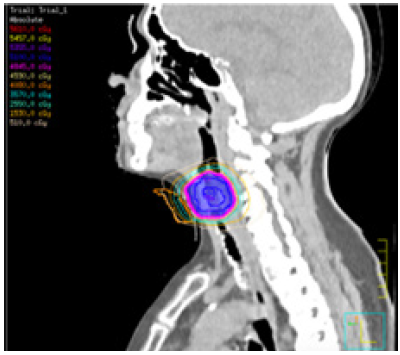
RT was delivered by nonconformal 2 dimensional (2D) or by IMRT/VMAT techniques. The patients who received 2D treatment were treated with conventional anatomic field borders as follows; (1) superior field edge was the thyroid notch (2) inferior field edge was below the thyroid cartilage (3) posterior field edge was 1cm posterior to the thyroid cartilage (4) the anterior field edge was 1cm anterior to the neck. Modulated radiation treatment delivery was either with VMAT or IMRT. Patients who received IMRT/VMAT underwent CT-based simulation and planning (i.e., delineating clinical target volume, planning target volume and conforming the beams to these volumes to minimize exposure of normal uninvolved tissue) (Figures 1 & 2). In the modulated radiotherapy setting, the VMAT technique was used in most of the cases after we transitioned following a brief period of IMRT to VMAT.
For patients which were treated with IMRT/VMAT, the gross tumor volume (GTV) was established based on radiologic imaging and the detailed description of disease from the time of consultation. The GTV was expanded by 5mm to create a clinical tumor volume (CTV) that typically excluded the contralateral arytenoid. The planning tumor volume (PTV) was planned with the intent of minimizing the dose to the carotid arteries, and submandibular glands. With both the historical techniques and our modern conformal techniques the dose remained constant at 5000- 5100 cGy in 20 fractions, over four weeks.
Figure 1 represents a historical 2-D using traditional field borders, whereas Figure 2 shows the PTV of a VMAT planned method.
Clinical Evaluations
At our institution, standard clinical follow-up for these patients occur every 3 months in the first and second year, every 6 to 12 months in years 3 to 5, and then when patients preferred ongoing evaluations, annually beyond 5 years. Each follow-up included a physical examination including direct or indirect nasopharyngoscopic examination. All patients reported in this cohort were followed for at least two years..
Data Collection
For all patients, the following data were retrived from the patient charts; age at the diagnosis, date of diagnosis, TNM classification, gender, duration of RT, fraction size and total radiation dose, treatment technique, date of recurrence, date of failure (defined as date of clinical, pathological or radiological recurrence), and date of last known contact with the patient or date of death
Analysis Plan
Descriptive statistics were used to summarize patient characteristics, treatments, and outcomes. The primary outcome was the local control rate, defined from the date of diagnosis until the date of local recurrence, which adjusted for the competing risk of death. Patients alive and without a local recurrence were censored on the date of last known follow-up. Secondary outcomes included locoregional-free survival, distant metastasis-free survival and overall survival. Cumulative incidence methods using the Fine and Gray method were used for local control, while the Kaplan- Meier method was used to estimate time-to-event outcomes. Cox proportional hazards regression was used to investigate factors prognostic of outcomes. Variables to be included in multivariable models were identified using forward stepwise selection. Given the small sample size, patients who had modulated radiation (IMRT or VMAT) were combined for analysis. Confidence intervals were provided for estimates of interest. All tests and confidence intervals were two-sided and statistical significance was defined at the alpha=0.05 level.
Results
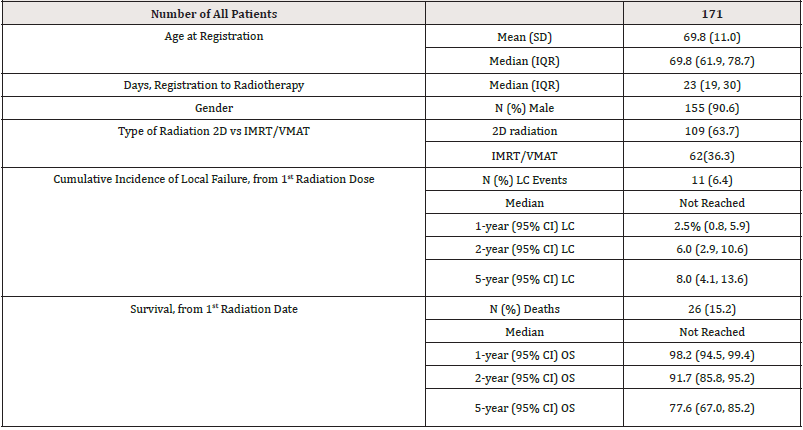
A total of 171 patients with T1 glottic cancer were treated with definitive RT alone and comprise the population of this study, see Table 1. The majority of patients (155) were male representing 90.6% of cases. The median patient age at the time of diagnosis was 69.8 years (range of 38-91 years). A total of 109 patients (63.7%) were treated with 2D techniques, whereas 62 patients (36.2%) were treated with IMRT/VMAT. Of these 62 patients, 18 (10.5%) were treated with IMRT, and 44 (25.7%) were treated with VMAT. Our center moved from 2D treatment to IMRT and then quickly evolved to VMAT; for the purpose of this analysis, we have pooled the data of IMRT and VMAT treatments together.
IMRT: Intensity Modulated Radiotherapy; VMAT: Volumetric Modulated arc Therapy; LC: Local Control, OS: Overall Survival
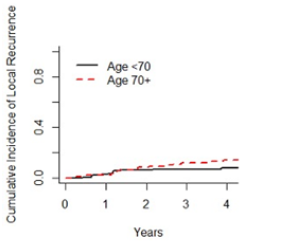
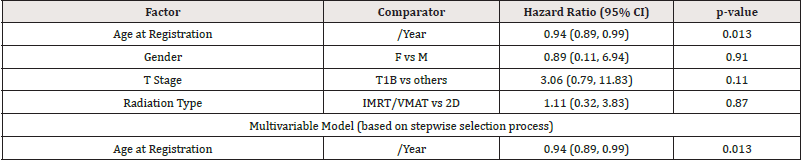
After a median follow up of over five years, there were only 11 patients (11/171 = 6.4%) that had documented local regional failure, most (9/11) occurring within the first year of follow up, see Figure 3. Of those 11 patients, six patients were in the 2D treatment group (6/109 = 5.5%), and five patients were in IMRT/VMAT group (5/62 = 8.1%). Age was the only factor which was observed to be significant prognostic factor (hazard ratio=0.94, 95% CI=0.89 to 0.99, p-value=0.013), see Table 2. After adjusting for age, no other factor was statistically significant, hence multivariable models were not reported. Figure 4 shows the cumulative incidence rates of patients categorized by age ≥70 versus <70. Of those <70, the 2-year cumulative incidence of local failure was 8.0 % (95% CI 3.2% to 15.7%) compared with 3.9% (1.0% to 10.1%) for those 70 and older.
IMRT: Intensity Modulated Radiotherapy; VMAT: Volumetric Modulated arc Therapy; LC: Local Control; OS: Overall Survival
Salvage Treatment
All 11 patients with local failure underwent successful salvage in the form of total laryngectomy ± bilateral selective neck dissection (levels II to IV). Salvage attempts were considered successful if the patient survived at least 1 year after the procedure and remained disease free at the site of recurrence.
Overall Survival (OS)
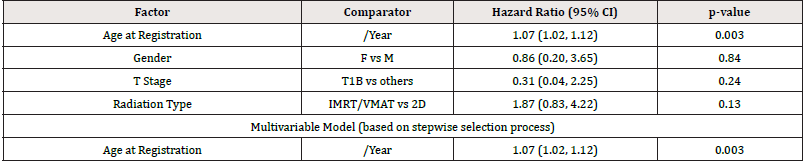
A total of 26 (15.2%) patients are known to have died. Five-year (95% CI) overall survival for this patient population was 77.6% (95% CI=67.0% to 85.2%). The only prognostic factor of OS was age (hazards ratio=1.07/year, 95% CI=1.02 to 1.12, p-value=0.003), see Table 3. Results were similar for other secondary outcomes (data not shown).
IMRT: Intensity Modulated Radiotherapy; VMAT: Volumetric Modulated arc Therapy
Discussion
At times the allure of technologic advances, and the rapid integration into routine clinical practice make the formal evaluation of these new techniques and treatment strategies difficult to perform. While the intuitive benefits are likely to exist, they may be difficult to measure or appreciate. With early-stage larynx cancer, it is not clear that most of our patients have less acute toxicity with newer RT techniques, nor is it clear that voice quality has improved, but for the average patient this is likely the case. Perhaps even more important however is the need to ensure that there are not measurable risks with the new techniques of RT, and in particular that a more focused approach to target delineation has not resulted in a higher rate of local disease failure or recurrence. We must recognize that excellent rates of local control existed with what appears in an historical context to be more rudimentary.
Our study does not reveal any concerns with the disease control of our newer radiation treatment techniques (IMRT/VMAT). There was no difference in survival of patients in 2D versus IMRT/VMAT treatment techniques. This is consistent with previous studies [15]. Equally, a local control rate that has remained well above 90% is consistent with other modern series also looking to ensure success with the shift to IMRT and VMAT.
There is little doubt that newer conformal radiation delivery can reduce the dose to carotid arteries, recent studies also confirm this effect [13,14] but the absolute benefit may only be visible with large population based registries akin to the potentially damaging effects of breast radiation to the lungs and cardiac outcomes.
But like all retrospective reviews, there are significant limitations with the collection of acute and late sequelae of radiation therapy. Whether the prospective collection of such data is warranted at this point, given the shift to the routine use of IMRT/ VMAT in radiation can be debated.
With a closer look at the failure pattern in this study we understand that most of our failures occurred during the first year after treatment. we think that this could be base for more detailed studies evaluating the need and intensity of post radiation follow up.
While this report provides the clinical outcomes on a relatively large number of patients, its design has limitations, foremost of which is that it is a non-randomized retrospective analysis. We have previously noted the inability to understand the impact of the different treatment techniques on the quality of life or acute toxicity metrics of our patients as it was not consistently collected in real time. The rate of local disease failure is also relatively low, limiting the statistical power of any comparisons between the two groups of patients. Fortunately, there were no other changes in the management of our patients over the time period selected. Staging CT scans of the neck for example were relatively rare over this period of time, and no changes to dose or fractionation occurred. The collection of disease outcomes was independent of treatment techniques, but clearly there was a temporal relationship difficult not to appreciate. We will continue to monitor our treatment outcomes for this population of patients, as it may well represent a simple surrogate for the quality of our radiation program for head and neck cancer in general.
Conflict of Interest
Authors declare no conflict of interest with this manuscript.
References
- Waldfahrer F, Hauptmann HB (2005) [Lymph node metastasis of glottic laryngeal carcinoma]. Laryngorhinootologie 84(2): 96-100.
- Lim YJ, Wu HG, Kwon TK, Hah JH, Sung MW, et al. (2015) Long-Term Outcome of Definitive Radiotherapy for Early Glottic Cancer: Prognostic Factors and Patterns of Local Failure. Cancer Res Treat 47(4): 862-870.
- Hartl DM, Ferlito A, Brasnu DF, Langendijk JA, Rinaldo A, et al. (2011) Evidence-based review of treatment options for patients with glottic cancer. Head Neck 33(11): 1638-1648.
- Forastiere AA, Ismaila N, Lewin JS, Nathan CA, Adelstein DJ, et al. (2018) Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 36(11): 1143-1169.
- Mendenhall WM, Amdur RJ, Morris CG, Hinerman RW (2001) T1-T2N0 squamous cell carcinoma of the glottic larynx treated with radiation therapy. J Clin Oncol 19(20): 4029-4036.
- Wong JR (1998) Radiation Therapy for Head and Neck Neoplasms. Wang CC (Ed.), Clinical Imaging, J Wiley, New York, USA, pp. 387.
- Warde P, O'Sullivan B, Bristow RG, Panzarella T, Keane TJ, et al. (1998) T1/T2 glottic cancer managed by external beam radiotherapy: the influence of pretreatment hemoglobin on local control. Int J Radiat Oncol Biol Phys 41(2): 347-353.
- Gupta T, Agarwal J, Jain S, Phurailatpam R, Kannan S, et al. (2012) Three-dimensional conformal radiotherapy (3D-CRT) versus intensity modulated radiation therapy (IMRT) in squamous cell carcinoma of the head and neck: a randomized controlled trial. Radiother Oncol 104(3): 343-348.
- Gupta T, Sinha S, Ghosh-Laskar S, Budrukkar A, Mummudi N, et al. (2020) Intensity-modulated radiation therapy versus three-dimensional conformal radiotherapy in head and neck squamous cell carcinoma: long-term and mature outcomes of a prospective randomized trial. Radiat Oncol 15(1): 218.
- Felice FDE, Pranno N, Papi P, Brugnoletti O, Tombolini V, et al. (2020) Xerostomia and Clinical Outcomes in Definitive Intensity Modulated Radiotherapy (IMRT) Versus Three-dimensional Conformal Radiotherapy (3D-CRT) for Head and Neck Squamous Cell Carcinoma: A Meta-analysis. In Vivo 34(2): 623-629.
- Chera BS, Amdur RJ, Morris CG, Mendenhall WM (2010) Carotid-sparing intensity-modulated radiotherapy for early-stage squamous cell carcinoma of the true vocal cord. Int J Radiat Oncol Biol Phys 77(5): 1380-1385.
- Feigenberg SJ, Lango M, Nicolaou N, Ridge JA (2007) Intensity-modulated radiotherapy for early larynx cancer: is there a role? Int J Radiat Oncol Biol Phys 68(1): 2-3.
- Mohamed ASR, Smith BD, Smith JB, Sevak P, Malek JS, et al. (2020) Outcomes of carotid-sparing IMRT for T1 glottic cancer: Comparison with conventional radiation. Laryngoscope 130(1): 146-153.
- Zumsteg ZS, Riaz N, Jaffery S, Hu M, Gelblum D, et al. (2015) Carotid sparing intensity-modulated radiation therapy achieves comparable locoregional control to conventional radiotherapy in T1-2N0 laryngeal carcinoma. Oral Oncol 51(7): 716-723.
- Wegner RE, Abel S, Bergin JJ, Colonias A (2020) Intensity-modulated radiation therapy in early stage squamous cell carcinoma of the larynx: treatment trends and outcomes. Radiat Oncol J 38(1): 11-17.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.